The bioactivity of oxybenzone—a harmful chemical often found in sunscreens—was examined within mouse models of breast cancer in high- and low-fat dietary contexts.

Oxybenzone (benzophenone-3; BP-3) is a toxic endocrine-disrupting chemical (EDC). Alarmingly, this chemical has been identified as a common ingredient in some brands of sunscreen. Oxybenzone can often be found in humans, household dust, fish and, due to its widespread human use, the water environment—causing harm to coral reefs and other murine life. Previous studies have shown that environmental toxins and estrogenic chemicals have emerged as potential culprits in the promotion of breast cancer. Furthermore, oxybenzone has been known to have estrogenic and anti-estrogenic properties.
“Although BP-3 has a very short half-life, its presence is widespread in human urine [9], in as much as 98% of the general U.S. population [13].”
Researchers from the Breast Cancer and the Environment Research Program at Michigan State University studied the diet-dependent effects of oxybenzone in mouse models of mammary tumorigenesis during puberty and adulthood. Their paper was published by Oncotarget in 2020, and entitled, “Benzophenone-3 promotion of mammary tumorigenesis is diet-dependent.”
“We [previously] demonstrated enhancement of mammary tumorigenesis by a diet high in saturated animal fat (HFD) [5–8]. Thus, examination of the activity of EDCs in a dietary context may provide additional insight into the potential role of EDCs in promoting breast cancer.”
The Study
In the current study, the team employed the Trp53–null transplantation of a basal-like breast cancer mouse model. The researchers previously demonstrated that proliferative, inflammatory and angiogenic activity in the mammary gland can be modulated by estrogen and a high-fat diet (HFD). Therefore, both pubertal and adult mice were placed on either low- or high-fat diets. After one week, study mice were ovariectomized, given time for recovery and the natural dissipation of endogenous hormones, and then treated for five days with either saline (control) or 17β-estradiol (E2).
Next, the estrogenic or anti-estrogenic effects of oxybenzone were examined in these mice under three dietary conditions: mice fed a life-long low-fat diet (LFD), mice fed a LFD during puberty and then a HFD in adulthood (LFD-HFD) and finally, mice fed a HFD during puberty and then a LFD in adulthood (HFD-LFD). Mice in LFD-HFD and HFD-LFD groups were fed their initial diet from three to 10 weeks of age, and were then switched to the alternative diet. Half of these mice were injected with oxybenzone and the other half (control) were injected with saline.
“We found that BP-3 had complex effects that were dependent upon dietary regimen and tumor histopathology.”
Results
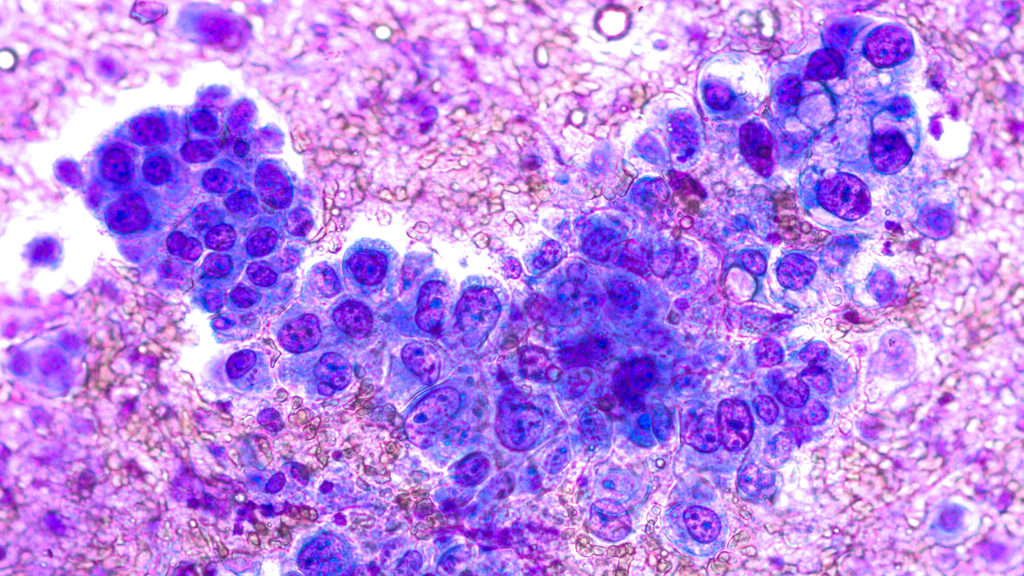
Consistent with their previous studies, the researchers found that most of the tumors developed were epithelial in histological composition, and few were spindle cell carcinomas. They found that oxybenzone reduced the tumorigenesis of epithelial tumors in LFD mice. The LFD-HFD combination resulted in more spindle cell tumors compared to the life-long LFD mice. Oxybenzone treatment increased the tumorigenesis of epithelial tumors in mice fed the LFD-HFD.
“Kaplan-Meier analysis revealed that BP-3 reduced tumorigenesis of epithelial tumors in mice fed LFD (Figure 3A). On the other hand, consistent with the increased proportion of epithelial tumors, BP-3 was promotional for epithelial tumorigenesis in mice fed LFD-HFD (Figure 3C), while reducing spindle cell tumorigenesis (Figure 3D).”
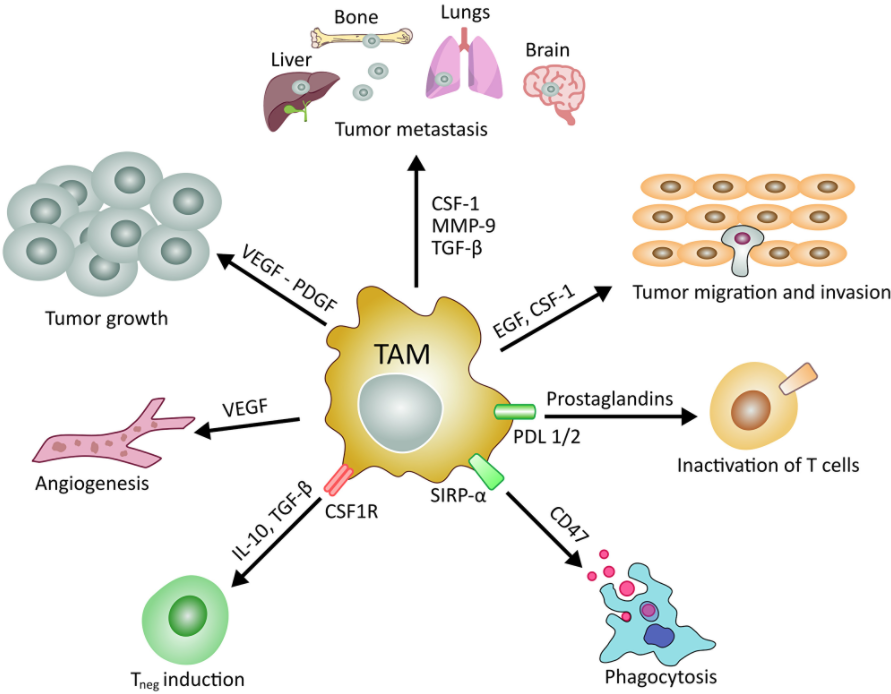
Researchers saw that proliferation was increased by oxybenzone treatment most significantly in the mammary glands of 26-week-old HFD mice. Curiously, oxybenzone treatment increased the number of lesions only in mice fed the HFD-LFD. The researchers note that, in this study and others, a “pubertal window of susceptibility” was observed, reinforcing the important notion that puberty is a highly sensitive window of time for poor diets and adverse exposures to environmental toxins. Ultimately, the team found that oxybenzone enhances estrogen-stimulated breast cancer cell proliferation in pubertal mice fed a HFD.
“Benzophenone-3 increased tumor cell proliferation, decreased tumor cell apoptosis, and increased tumor vascularity dependent on specific dietary regimen and tumor histopathology.”
Conclusion
Collectively, the researchers’ findings suggest that exposure to oxybenzone has adverse consequences in mammary tumorigenesis. The degree of severity appeared to be modulated differently among the three dietary regimens studied. Mice fed a HFD in adulthood experienced a decrease in tumor cell apoptosis and an increase in tumor vascularity and tumor cell proliferation. They note that there is future value in exploring the differences between pubertal and adult exposure to oxybenzone on a constant diet regimen.
“This points to a need for further studies of benzophenone-3 in both animal models and humans as a potential breast cancer risk factor, as well as a more general need to evaluate endocrine disrupting chemicals in varying dietary contexts.”
Click here to read the full scientific study, published by Oncotarget.
YOU MAY ALSO LIKE: More Oncotarget Videos on LabTube
—
Oncotarget is a unique platform designed to house scientific studies in a journal format that is available for anyone to read without a paywall making access more difficult. This means information that has the potential to benefit our societies from the inside out can be shared with friends, neighbors, colleagues, and other researchers, far and wide.
For media inquiries, please contact media@impactjournals.com.