Crossref is a non-profit organization that logs and updates citations for scientific publications. Each month, Crossref identifies a list of the most popular Oncotarget papers based on the number of times a DOI is successfully resolved.

DOI: https://doi.org/10.18632/oncotarget.28088
Author: Yuri Lazebnik
Institution: Lerna Consulting
Quote: “A distinctive feature of the SARS-CoV-2 spike protein is its ability to efficiently fuse cells, thus producing syncytia found in COVID-19 patients. This commentary proposes how this ability enables spike to cause COVID-19 complications as well as side effects of COVID-19 vaccines, and suggests how these effects can be prevented.”
DOI: https://doi.org/10.18632/oncotarget.24807
Authors: Sandra Rosskopf, Judith Leitner, Wolfgang Paster, Laura T. Morton, Renate S. Hagedoorn, Peter Steinberger, and Mirjam H.M. Heemskerk
Institutions: Medical University of Vienna and Leiden University Medical Center
Quote: “Adoptive T cell therapy using TCR transgenic autologous T cells has shown great potential for the treatment of tumor patients. Thorough characterization of genetically reprogrammed T cells is necessary to optimize treatment success. Here, we describe the generation of triple parameter reporter T cells based on the Jurkat 76 T cell line for the evaluation of TCR and chimeric antigen receptor functions as well as adoptive T cell strategies.”
DOI: https://doi.org/10.18632/oncotarget.13196
Authors: Rui Liu, Chengyong Tang, Ai Shen, Huating Luo, Xufu Wei, Daofeng Zheng, Chao Sun, Zhongtang Li, Di Zhu, Tingting Li, and Zhongjun Wu
Institution: The First Affiliated Hospital of Chongqing Medical University
Quote: “IL-37 has been characterized as a fundamental inhibitor of innate immunity and a tumor suppressor in several cancers. However, the molecular mechanism of IL-37 in hepatocellular carcinoma (HCC) is largely unclear. In this study we found IL-37 expression was down-regulated in human HCC tissues and cell lines, and was negatively correlated with tumor size, vascular invasion, as well as overall-survial and disease-free survival (OS and DFS) of HCC.”
DOI: https://doi.org/10.18632/oncotarget.25989
Authors: Xiaofeng Li, Yueming He, Jinfeng Zhu, Hongxia Pang, Yongwei Lin, and Jinyang Zheng
Institution: Affiliated Quanzhou First Hospital of Fujian Medical University
Quote: “Sarcomatoid carcinoma is a rare malignancy characterized by a combination of epithelial and sarcoma or sarcoma-like components. In this study, we reported one case of pulmonary sarcomatoid carcinoma and evaluated the safety and efficacy of apatinib, a tyrosine kinase inhibitor selectively targeting vascular endothelial growth factor receptor 2, in treating this disease.”
#6: Treasures from trash in cancer research
DOI: https://doi.org/10.18632/oncotarget.28308
Authors: Fabiano Cordeiro Moreira, Dionison Pereira Sarquis, Jorge Estefano Santana de Souza, Daniel de Souza Avelar, Taíssa Maria Thomaz Araújo, André Salim Khayat, Sidney Emanuel Batista dos Santos, and Paulo Pimentel de Assumpção
Institutions: Universidade Federal do Pará and Universidade Federal do Rio Grande do Norte
Quote: “Cancer research has significantly improved in recent years, primarily due to next-generation sequencing (NGS) technology. Consequently, an enormous amount of genomic and transcriptomic data has been generated. In most cases, the data needed for research goals are used, and unwanted reads are discarded. However, these eliminated data contain relevant information. Aiming to test this hypothesis, genomic and transcriptomic data were acquired from public datasets.”
DOI: https://doi.org/10.18632/oncotarget.28178
Authors: Connor Willis, Hillevi Bauer, Trang H. Au, Jyothi Menon, Sudhir Unni, Dao Tran, Zachary Rivers, Wallace Akerley, Matthew B. Schabath, Firas Badin, Ashley Sekhon, Malini Patel, Bing Xia, Beth Gustafson, John L. Villano, John-Michael Thomas, Solomon J. Lubinga, Michael A. Cantrell, Diana Brixner, and David Stenehjem
Institutions: University of Utah, University of Minnesota Duluth, Huntsman Cancer Institute, H. Lee Moffitt Cancer Center and Research Institute, Baptist Health Medical Group, MetroHealth Medical Center, Rutgers Cancer Institute of New Jersey, University of Southern California, Saint Luke’s Cancer Institute, University of Kentucky, and Bristol Myers Squibb
Quote: “Tumor mutational burden (TMB) is a potential biomarker to predict tumor response to immuno-oncology agents in patients with metastatic non-small cell lung cancer (NSCLC). A multi-site cohort study evaluated patients diagnosed with stage IV NSCLC between 2012 and 2019 who had received comprehensive genomic profiling (CGP) and any NSCLC-related treatment at 9 U.S. cancer centers. Baseline characteristics and clinical outcomes were compared between patients with TMB <10 and TMB ≥10.”
DOI: https://doi.org/10.18632/oncotarget.28249
Authors: Raquel Torres-Guzmán, Maria Patricia Ganado, Cecilia Mur, Carlos Marugan, Carmen Baquero, Yanzhu Yang, Yi Zeng, Huimin Bian, Jian Du, Alfonso de Dios, Oscar Puig, and María José Lallena
Institution: Eli Lilly and Company
Quote: “Abemaciclib is an oral, selective cyclin-dependent kinase 4 & 6 inhibitor (CDK4 & 6i), approved for hormone receptor-positive (HR+), human epidermal growth factor receptor 2-negative (HER2–) advanced breast cancer (ABC) as monotherapy for endocrine refractory disease, and with endocrine therapy (ET) for initial treatment and after progression on ET. Abemaciclib has also shown clinical activity in combination with ET in patients with high risk early BC (EBC). Here, we examined the preclinical attributes of abemaciclib and other CDK4 & 6i using biochemical and cell-based assays. In vitro, abemaciclib preferentially inhibited CDK4 kinase activity versus CDK6, resulting in inhibition of cell proliferation in a panel of BC cell lines with higher average potency than palbociclib or ribociclib.”
#3: Increased gut permeability in cancer cachexia: mechanisms and clinical relevance
DOI: https://doi.org/10.18632/oncotarget.24804
Authors: Laure B. Bindels, Audrey M. Neyrinck, Audrey Loumaye, Emilie Catry, Hannah Walgrave, Claire Cherbuy, Sophie Leclercq, Matthias Van Hul, Hubert Plovier, Barbara Pachikian, Luis G. Bermúdez-Humarán, Philippe Langella, Patrice D. Cani, Jean-Paul Thissen, and Nathalie M. Delzenne
Institutions: Université Catholique de Louvain and Université Paris-Saclay
Quote: “Intestinal disorders often occur in cancer patients, in association with body weight loss, and this alteration is commonly attributed to the chemotherapy. Here, using a mouse model of cancer cachexia induced by ectopic transplantation of C26 cancer cells, we discovered a profound alteration in the gut functions (gut permeability, epithelial turnover, gut immunity, microbial dysbiosis) independently of any chemotherapy.”
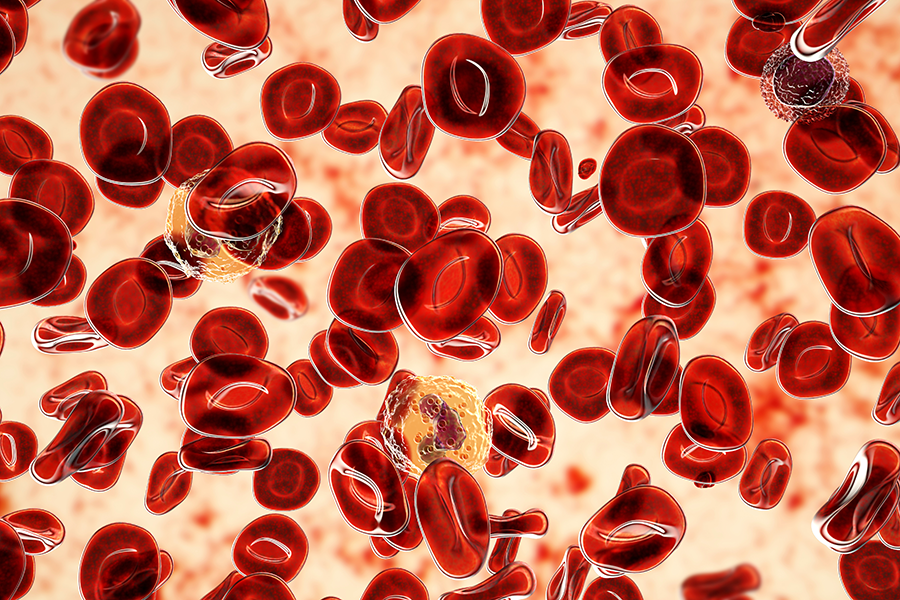
#2: Inflammatory responses and inflammation-associated diseases in organs
DOI: https://doi.org/10.18632/oncotarget.23208
Authors: Linlin Chen, Huidan Deng, Hengmin Cui, Jing Fang, Zhicai Zuo, Junliang Deng, Yinglun Li, Xun Wang, and Ling Zhao
Institution: Sichuan Agricultural University
Quote: “Inflammation is a biological response of the immune system that can be triggered by a variety of factors, including pathogens, damaged cells and toxic compounds. These factors may induce acute and/or chronic inflammatory responses in the heart, pancreas, liver, kidney, lung, brain, intestinal tract and reproductive system, potentially leading to tissue damage or disease. Both infectious and non-infectious agents and cell damage activate inflammatory cells and trigger inflammatory signaling pathways, most commonly the NF-κB, MAPK, and JAK-STAT pathways. Here, we review inflammatory responses within organs, focusing on the etiology of inflammation, inflammatory response mechanisms, resolution of inflammation, and organ-specific inflammatory responses.”
DOI: https://doi.org/10.18632/oncotarget.25146
Authors: Angie M. Y. Shum, Anne Poljak, Nicholas L. Bentley, Nigel Turner, Timothy C. Tan, and Patsie Polly
Institutions: UNSW Sydney, Western Clinical School and Westmead Hospital
Quote: “Cancer cachexia is observed in more than 50% of advanced cancer patients, and impairs quality of life and prognosis. A variety of pathways are likely to be dysregulated. Hence, a broad-spectrum understanding of the disease process is best achieved by a discovery based approach such as proteomics.”
Click here to read the latest papers published by Oncotarget in Volume 14.
ONCOTARGET VIDEOS: YouTube | LabTube | Oncotarget.com
—
Oncotarget is an open-access, peer-reviewed journal that has published primarily oncology-focused research papers since 2010. These papers are available to readers (at no cost and free of subscription barriers) in a continuous publishing format at Oncotarget.com. Oncotarget is indexed/archived on MEDLINE / PMC / PubMed.
For media inquiries, please contact media@impactjournals.com.